
Image Source: Canva
Fungal infections continue to be a chronic and widespread issue that impacts billions of people worldwide. The demand for efficient treatments has never been greater, given the size of the affected population. How well do fungus eliminators work to treat these resistant infections? This article explores the realm of fungus eliminators and looks at how well they work to treat these common health issues.
The Growing Concern about Fungal Infections
Fungal infections are more than just an annoyance; in some cases, they can result in serious sickness and greatly affect quality of life. Nail fungus, or onychomycosis, generally affects people, with a higher incidence among the elderly. Ringworm causes all fungal-related skin diseases globally.
Common Fungal Infections: A Closer Look
Before we dive into treatments, let’s examine the most prevalent fungal infections, like ringworm and fungal nail infections. Athlete’s Foot (Tinea Pedis) thrives in warm, moist environments, making feet particularly vulnerable. Symptoms include itching and burning between the toes, cracked, peeling skin, and redness and scaling on the soles.
Nail Fungus (Onychomycosis), affecting both fingernails and toenails, can be stubborn and long-lasting, manifesting as thickened nails, discoloration (yellow, brown, or white), and a brittle or crumbly nail texture. Ringworm (Tinea Corporis), despite its name, is a fungal infection, not a worm. It is characterized by circular, red, itchy patches on the skin, raised, scaly borders, and gradual spreading of the affected area.
How Fungus Eliminators Work: The Science Behind the Solution
These treatments, including both topical applications and oral medications, are formulated to disrupt fungal cell membranes or inhibit essential enzymes crucial for fungal growth. Clinical studies and research consistently highlight their efficacy in achieving significant cure rates for various fungal infections. For instance, the fungus eliminator Pure Health has been recognized for its effectiveness in clinical settings. By following recommended treatment protocols and maintaining good hygiene practices, individuals can effectively manage fungal infections and enhance their overall well-being.
Understanding all of the methods that fungus eliminators use to fight infections can help you select the best treatment for your situation. Antifungal creams, ointments, and solutions are instances of topical treatments that act directly on the affected region. Amorolfine, which breaks down fungal cell membranes, and ciclopirox, which prevents vital fungal enzymes from functioning, are common constituents.
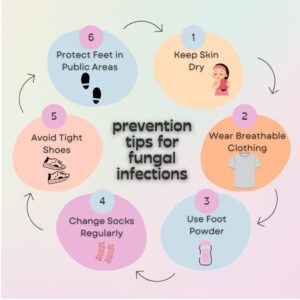
Image Source: Canva
Effectiveness of Fungus Eliminators: What the Studies Say
Clinical evidence offers significant details about how effective different therapies are. Terbinafine beat itraconazole to cure onychomycosis, according to a meta-analysis. For toenail onychomycosis, the Cochrane Review concluded that oral antifungal drugs, such as terbinafine at the top of the list, are more successful than topical therapies.
In addition, a double-blind study found that topical bifonazole treatment and urea nail ablation increased complete cure rates for nail fungus by an unbelievable amount. These results emphasize how crucial it is to select the right course of action depending on the particular infection and its severity.
Comparing Popular Fungus Eliminators
| Treatment | Type | Effectiveness | Best For | Side Effects | Treatment Duration: |
| Terbinafine | Oral | High (76% cure rate) | Nail fungus | Rare liver issues | 6-12 weeks |
| Itraconazole | Oral | Moderate (43% cure rate) | Various fungal infections | Potential drug interactions | 3-4 months |
| Ciclopirox | Topical | Moderate | Athlete’s foot, ringworm | Minimal (skin irritation) | 4-8 weeks |
| Amorolfine | Topical | Moderate to High | Nail fungus | Minimal (nail discoloration) | Up to 12 months |
| Urea + Bifonazole | Combination | Very High (414% increase in cure rate) | Severe nail fungus | Minimal | 2-4 weeks |
Advantages and Limitations of Fungus Eliminators
Fungus eliminators offer distinct advantages and considerations. They are widely accessible, with many options available over the counter, providing convenience for users seeking immediate relief. These treatments also offer targeted solutions tailored to various types of fungal infections, ensuring effective management based on specific needs. Moreover, fungus eliminators are supported by rigorous scientific research and clinical studies, validating their efficacy and safety.
There are limitations to take into account, though. Treatment times can be long; months of regular application are necessary for certain illnesses before any improvement is shown. Despite their strength, oral drugs have the potential to cause adverse effects, the severity of which might vary from person to person.
In addition, the absence of suitable preventive measures may lead to a recurrence of illness, highlighting the importance of continued care and good hygiene habits. Understanding these benefits and drawbacks helps individuals select the most suitable treatment for their fungal infections.
Maximizing Treatment Effectiveness: Best Practices
It has been shown that fungus eliminators are powerful tools in the fight against fungus infections. Every kind and severity of infection has a treatment choice, ranging from potent oral drugs to topical therapies. The secret to success is selecting the best course of action, adhering to it spiritually, and taking preventive actions to stop recurrence. While many fungal infections can be treated with prescription drugs, severe or chronic cases should consult a doctor. You can get advice from a doctor about the best line of action for your specific situation.
The Future of Antifungal Treatments
Exciting developments are on the horizon in the field of antifungal treatments:
- Nanotechnology: Enhanced delivery systems are being developed to improve the effectiveness of topical treatments.
- Natural Compounds: Research into plant-based antifungals is underway, aiming to offer treatments with fewer side effects.
- Immunotherapy: Innovations are focusing on boosting the body’s natural defenses against fungal infections. These advancements promise more effective and patient-friendly treatments in the coming years, potentially revolutionizing the management of fungal infections.
Frequently Asked Questions
What is the best treatment for a fungal infection?
The best treatment for a fungal infection depends on the type and severity of the infection. Typically, antifungal medications—either topical creams or oral pills—are prescribed. It’s essential to follow your healthcare provider’s recommendations for dosage and duration.
What are antifungal agents effective against?
Antifungal agents are effective against a wide range of fungal infections, including athlete’s foot, nail fungus (onychomycosis), ringworm, and candidiasis (yeast infections). They work by targeting specific aspects of fungal cell structure or function, inhibiting growth and promoting healing.
How infection by fungi can be prevented and treated?
Preventing fungal infections involves maintaining good hygiene, such as keeping skin clean and dry, wearing breathable clothing, and avoiding sharing personal items. Treatment includes antifungal medications prescribed by a healthcare provider, tailored to the type and location of the infection.
How do you get rid of a fungal infection permanently?
Permanently eliminating a fungal infection often requires consistent treatment adherence and lifestyle adjustments. Antifungal medications, both topical and oral, are commonly used. Preventive measures, such as maintaining good hygiene and avoiding environments conducive to fungal growth, can help reduce recurrence risks.
Conclusion
It has been shown that fungus eliminators are powerful tools in the fight against fungus infections. Every kind and severity of infection has a treatment choice, ranging from potent oral drugs to topical therapies. The secret to success is selecting the best course of action, adhering to it religiously, and taking preventative measures to stop recurrence. While many fungal infections can be treated with prescription drugs, severe or chronic cases should consult a doctor. You can get advice from your healthcare practitioner about the best line of action for your specific situation. Act Now! Avoid letting fungus infections endanger your overall health and well-being.





